New COVID Variant 'Nimbus' Spreads in U.S., Linked to 'Razor Blade Throat'
Nimbus is rapidly increasing its presence across the United States. According to the CDC, the NB.1.8.1 variant now accounts for more than one-third of COVID-19 cases nationally.

AI Research Assistant
Analyze this article instantly
A new nickname is circulating in discussions about COVID-19, sparking concern: "razor blade throat." This unusually intense symptom is indeed associated with a rapidly spreading new variant, Nimbus, and it is certainly grabbing attention across the United States.
While the vivid description sounds alarming, experts are providing important insights. Despite the dramatic symptom, authoritative sources consistently report that the variant is not causing more severe overall illness or increased mortality. This article breaks down what Nimbus is, its characteristic symptoms, its spread, and what it means for public health.
What is Nimbus? Official Name and WHO Classification
The variant gaining notoriety for its distinctive symptom is informally known as Nimbus. Its official scientific designation is NB.1.8.1. This variant is a subvariant of the Omicron lineage of the SARS-CoV-2 virus, which causes COVID-19.
The World Health Organization (WHO) has classified Nimbus as a "variant under monitoring". This means it is under close observation due to characteristics like transmissibility.
It is not currently considered a "variant of concern," which would imply a higher public health risk.
Nimbus Rapidly Spreading Across U.S.
![]()
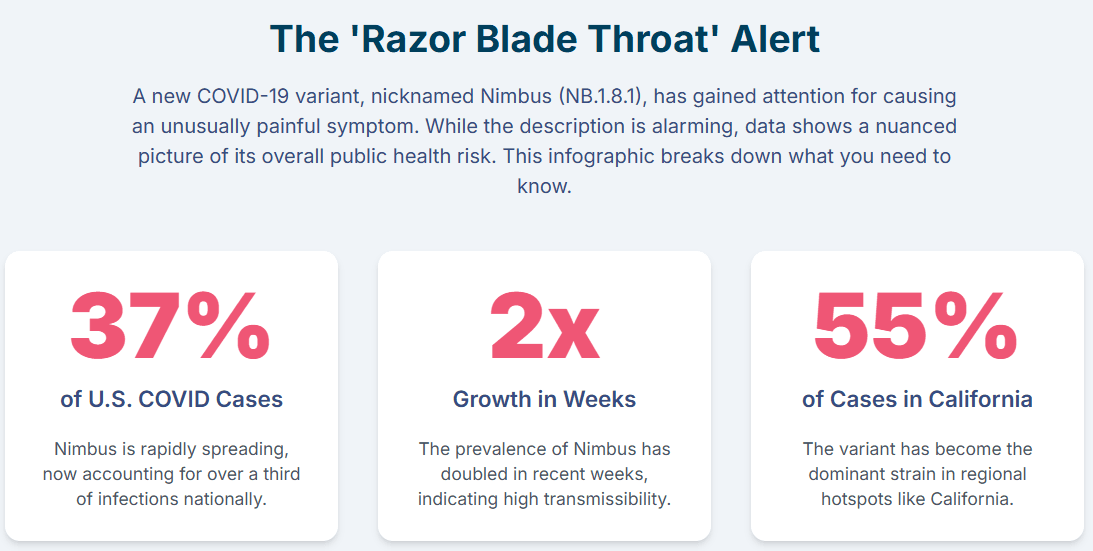
Nimbus is rapidly increasing its presence across the United States. According to the Centers for Disease Control and Prevention (CDC), the NB.1.8.1 variant now accounts for more than one-third of COVID-19 cases nationally.
More specifically, it represents 37% of COVID infections in Americans, a rate that has doubled in recent weeks. Health experts anticipate that Nimbus is on track to become the dominant strain in the country.
The variant has established a significant foothold in specific regions, particularly California. There, it now comprises 55% of detected COVID-19 cases. Wastewater surveillance in California has also indicated rising viral levels, an early warning sign of increasing community transmission.
The initial detection of Nimbus in the U.S. occurred through airport screening programs. These screenings identified the new covid variant in travelers arriving from regions such as the Eastern Mediterranean, Southeast Asia, and the Western Pacific. Cases were confirmed in California, Washington state, Virginia, and New York.
The consistent reporting of Nimbus rapidly increasing its proportion of cases in the U.S. suggests a significant growth advantage. This implies the variant is more transmissible or better at evading prior immunity.
The rapid rise in prevalence, even if overall case numbers are currently low , underscores the virus's ongoing evolutionary capacity. This highlights the continued importance of robust surveillance and public health measures.
The 'Razor Blade Throat' Phenomenon
'Razor Blade Throat': What It Feels Like
The symptom that has given the Nimbus variant its striking nickname is an unusually intense and excruciating sore throat. Patients describe the sensation as feeling like "swallowing razor blades" or "broken glass".
This severe discomfort can significantly hinder basic activities. These include talking, swallowing, eating, and staying hydrated. Even sips of water can be incredibly painful.
Typically, the severe sore throat associated with Nimbus lasts about a week. This symptom has become a focal point of public concern.
Is 'Razor Blade Throat' Unique to Nimbus?
It is important to note that a sore throat has long been a common and recognized symptom of COVID-19 across various variants. Up to 70% of COVID infections can include a sore throat.
While the "razor blade throat" has garnered significant attention, some experts offer a nuanced perspective. Dr. Scott Roberts of Yale School of Medicine indicates that the term is largely anecdotal.
There is not yet definitive evidence to suggest that this variant alone leads to a more severe sore throat than all other prior variants.
Nevertheless, the widespread and intense reports from patients infected with Nimbus have undeniably brought this symptom to the forefront. This highlights its severity in many cases.
There is a divergence in reports regarding the "uniqueness" of the razor blade throat. Public and media accounts heavily emphasize the symptom's distinct and severe nature for Nimbus. Patients describe it in extreme terms.
Conversely, a Yale expert states it is "anecdotal" and lacks evidence for more severe sore throat than other variants. This suggests that while the
reported experience of severity is high, the clinical data might not yet definitively prove a unique physiological mechanism.
Other Common Symptoms Associated with Nimbus
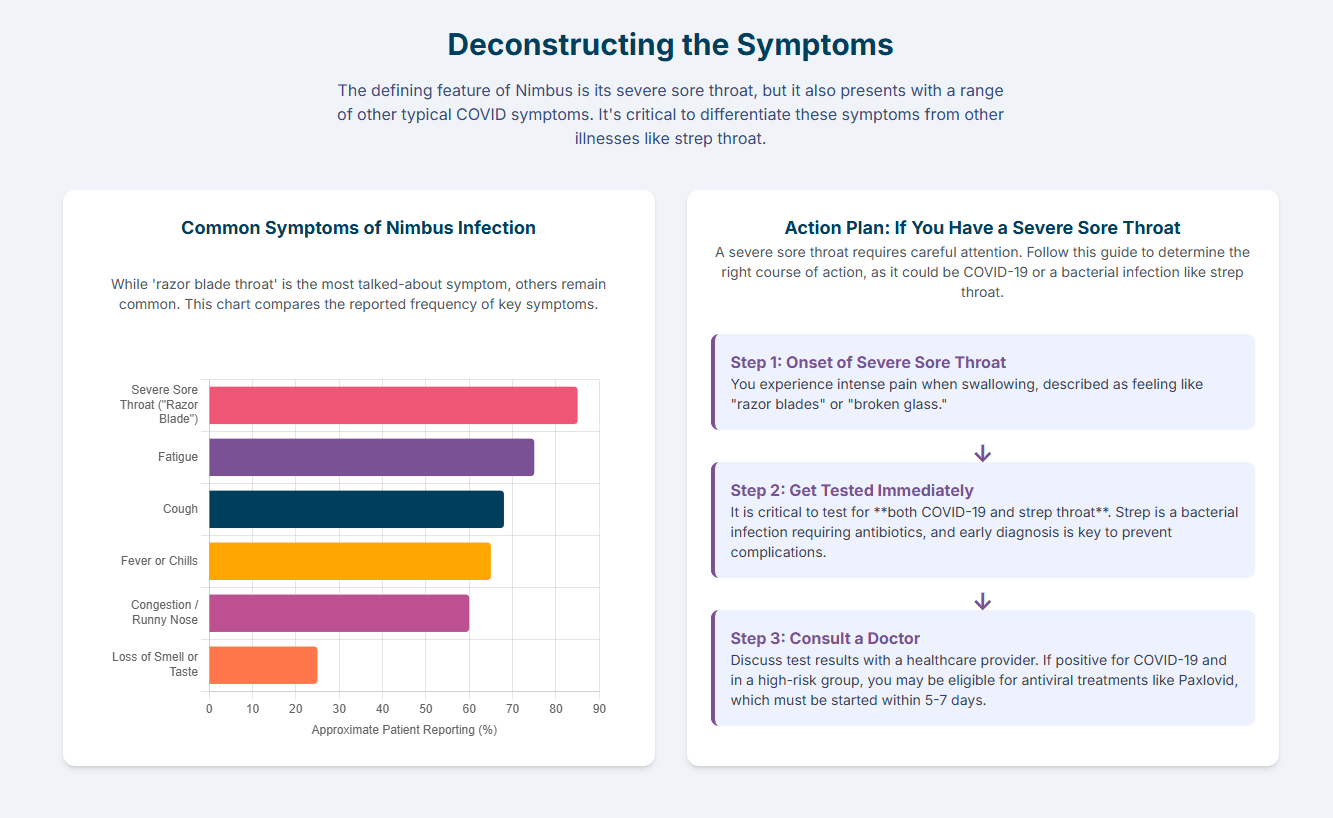
Beyond the distinctive sore throat, a Nimbus infection can present with a full spectrum of covid symptoms. These are largely consistent with other COVID-19 variants.
These include: fever, chills, cough, shortness of breath, loss of taste or smell, congestion, runny nose, fatigue, muscle or body aches, headache, nausea or vomiting, and diarrhea.
Less common symptoms can also occur. These include a skin rash, discolouration of fingers or toes, and red or irritated eyes.
Understanding Severity and Risk
Nimbus: Low Severity Despite Intense Symptoms
Despite the alarming "razor blade throat" symptom, health organizations and experts consistently report that the Nimbus variant is generally not causing more severe illness. This includes the WHO and CDC.
It is also not causing increased hospitalizations or higher mortality rates compared to previous COVID-19 variants.
This assessment is reinforced by medical professionals. Dr. Ahmed Salem, a pulmonologist at Sharp Memorial Hospital, stated, "Fortunately, it's actually less virulent so far. We're not seeing an increased mortality or increased death."
He also noted that hospital and ICU admissions for COVID-19 remain low. This is a positive indicator of the variant's overall impact on severe disease. While one report used the term "deadly subvariant" , it is important to contextualize this with the broader expert consensus on low severity.
Vaccines Remain Effective Against Nimbus
A critical piece of reassuring news is that current COVID-19 vaccines are expected to remain effective. They prevent severe disease, hospitalization, and death against the Nimbus variant.
The WHO has designated Nimbus as a "variant under monitoring" and considers the public health risk low at the global level. Current vaccines are expected to remain effective.
Further supporting this, Dr. Kartik Cherabuddi noted that early and limited laboratory data do "not show a significant capability to evade the immune system or increased resistance to antiviral treatment".
There is a subtle but important point regarding immune evasion. One source explicitly states that "early and limited laboratory data do not show a significant capability to evade the immune system or increased resistance to antiviral treatment" for Nimbus. This directly supports the effectiveness of vaccines against severe disease.
However, another source mentions "high immune evasion". This apparent discrepancy is important to clarify. The consensus from major health organizations like the WHO and multiple experts points to a low public health risk and continued vaccine effectiveness against severe outcomes. The "high immune evasion" mentioned might refer to evasion of
prior infection immunity or vaccine-induced immunity against mild infection or transmission, rather than evasion of protection against severe disease.
What to Do If You Experience Symptoms
Testing is Key for COVID and Strep Throat
If symptoms appear, it is advisable to get tested for COVID-19 immediately. This helps inform next steps, including potential treatment and preventing further spread.
Crucially, if an individual experiences a severe sore throat, it is vital to get tested for strep throat as well. This is particularly important to rule out a bacterial infection that requires antibiotic treatment.
Untreated strep throat can lead to serious complications. These include peritonsillar abscesses (pus-filled infections behind the tonsils), rheumatic fever (which can damage the heart, joints, and skin), and a type of kidney inflammation called post-streptococcal glomerulonephritis.
Managing Symptoms at Home
Most people with COVID-19, including those infected with the Nimbus variant, will experience mild illness. They can recover at home. For managing symptoms, several strategies can provide relief.
Getting plenty of rest is crucial to aid recovery. Drink ample fluids such as water, herbal teas, or broths to prevent dehydration. This is especially critical when severe throat pain makes swallowing difficult.
Use over-the-counter medications like acetaminophen (paracetamol) or ibuprofen. These can alleviate throat pain, reduce fever, and decrease inflammation.
Employ warm saltwater gargles, throat lozenges, and lidocaine sprays to soothe the throat. These provide temporary relief from the intense pain.
Using a humidifier can add moisture to the air, which helps prevent the throat from becoming dry and irritated. A teaspoon of honey can help with coughs, though honey should not be given to babies under 12 months.
If experiencing breathlessness, try turning down the heating, opening a window, breathing slowly in through the nose and out through the mouth. Sitting upright, relaxing shoulders, and leaning slightly forward can also help.
When to Seek Medical Help
The strong emphasis on differentiating "razor blade throat" from strep throat is a critical public health message. Untreated strep throat can lead to severe, long-term complications like rheumatic fever and kidney inflammation.
This highlights that a severe symptom, even if associated with a viral infection, can mask a bacterial one requiring different, urgent treatment. The strict time window for COVID antiviral treatments (5-7 days) for high-risk individuals underscores that early testing and medical consultation are vital.
It is crucial to note that these treatments must be started within 5-7 days of when symptoms first begin to be effective. Prompt consultation with a healthcare provider is essential if an individual is in a high-risk group.
Protecting Yourself and Others: Prevention Strategies
Key Prevention Strategies
To protect oneself and others from COVID-19, core prevention strategies remain essential. These are recommended by leading public health organizations like the CDC and WHO.
Staying up-to-date with COVID-19 vaccines remains a cornerstone of protection. While vaccinated individuals can still get infected, vaccination significantly lowers the risk of getting very sick, being hospitalized, or dying from COVID-19.
Practice diligent hand hygiene by frequently cleaning hands with alcohol-based hand rub or soap and water. Always cover the mouth and nose with a bent elbow or tissue when coughing or sneezing, disposing of used tissues immediately. Additionally, clean and disinfect frequently touched surfaces regularly.
Take steps to ensure cleaner air, especially indoors. This includes opening windows to bring in outdoor air, increasing air filtration (e.g., using portable HEPA cleaners), and turning on exhaust fans. When possible, opt for outdoor activities over indoor ones, as viral particles spread less readily outdoors.
The WHO advises avoiding the "3 Cs": spaces that are Closed, Crowded, or involve Close contact. These settings carry higher risks of transmission.
Isolation and Precautions
If respiratory symptoms develop or an individual tests positive for COVID-19, it is crucial to stay home. Avoid contact with others, including household members who are not sick.
Follow current CDC recommendations for isolation. Generally, this means staying home for at least 5 days if an individual is 18 or older, and for 3 days if under 18, after symptom onset or a positive test. It is recommended to continue wearing a high-quality mask when indoors around others for an additional 5 days after the isolation period.
Wear a properly fitted mask when physical distancing is not possible, in poorly ventilated settings, or when indoors around others after exposure or during the post-isolation period.
If an individual is at higher risk for severe illness, it is important to seek healthcare promptly for testing and/or treatment as soon as symptoms begin.
Public health messaging from the WHO and CDC increasingly emphasizes core prevention strategies and proactive health measures. Campaigns like "No one knows your risk like you do" indicate a shift towards empowering individuals to assess personal risk.
This approach encourages individuals to take appropriate, voluntary actions. It reinforces personal agency in navigating ongoing public health challenges.
Explore Funding Opportunities
Staying Informed and Protected
The Nimbus variant (NB.1.8.1) is a highly transmissible Omicron subvariant rapidly spreading in the U.S. It is notable for its intensely painful "razor blade throat" symptom.
While the throat pain can be excruciating, experts generally agree that Nimbus does not cause more severe overall illness, increased hospitalizations, or higher mortality rates. Crucially, current COVID-19 vaccines remain effective in preventing severe disease.
Core prevention strategies—staying up-to-date on vaccinations, practicing good hygiene, improving ventilation, and staying home when sick or exposed—are still vital and effective. Prompt testing (for both COVID-19 and strep throat) and seeking medical advice for severe or concerning symptoms are essential.
As COVID-19 continues to evolve, staying informed and taking proactive, evidence-based steps empowers individuals. By understanding variants like nimbus and applying proven public health strategies, we can collectively navigate the ongoing landscape of respiratory viruses with confidence and knowledge.




