Smarter Healthcare How AI is Changing the Future of Medicine
AI transforms healthcare with diagnostic precision and workflow efficiency but faces challenges like bias, transparency, and regulation, demanding ethical collaboration for equitable adoption

AI Research Assistant
Analyze this article instantly
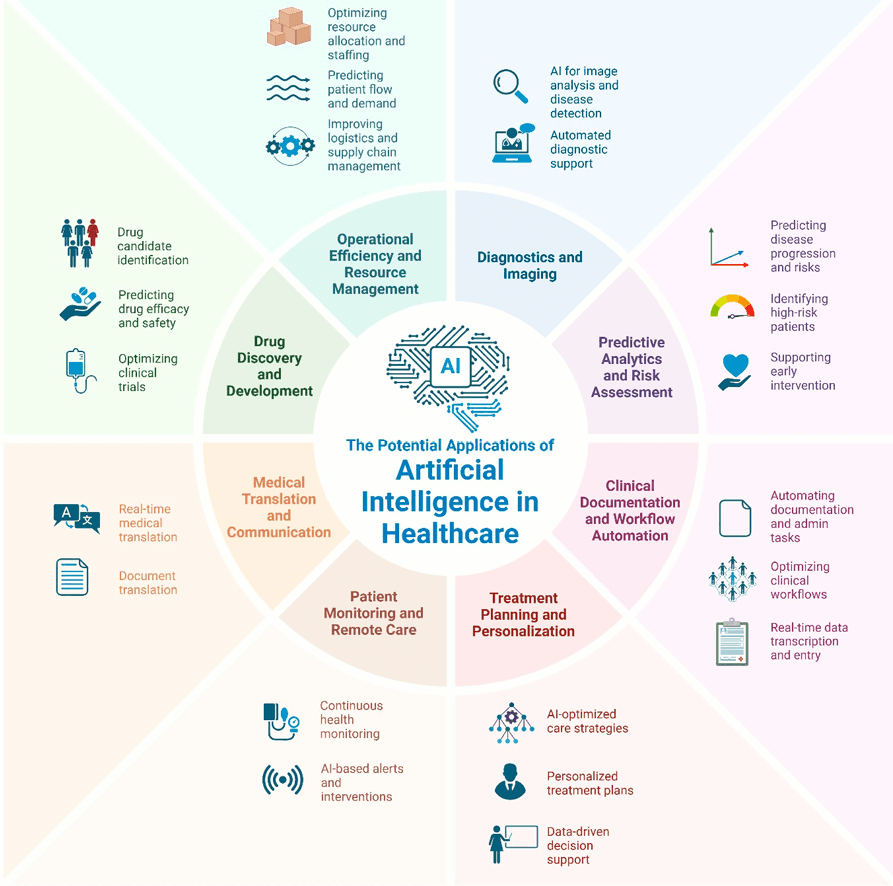
Artificial intelligence (AI) rapidly transforms healthcare, offering groundbreaking tools to improve accuracy, efficiency, and accessibility. From diagnosing diseases to streamlining workflows, AI is no longer a futuristic concept—it is actively reshaping how clinicians care for patients. However, realizing its full potential requires addressing critical challenges, from ethical dilemmas to systemic biases, to ensure these technologies benefit everyone.
AI in Diagnostics
AI’s impact is already visible in diagnostics. Advanced AI systems, such as deep learning models, now match human experts in tasks like identifying skin cancer or analyzing thyroid ultrasound images. These tools enhance precision and make specialized care more accessible, particularly in regions with limited medical resources.
Beyond diagnosis, AI-driven predictive analytics offer personalized insights, such as forecasting outcomes for colorectal cancer patients, outperforming traditional methods. In emergency settings, AI assistants like ChatGPT provide rapid support, suggesting diagnoses and treatment strategies to guide decision-making.
Clinical Workflow
AI is also revolutionizing clinical workflows. Generative AI automates time-consuming tasks, such as drafting medical notes, freeing clinicians to focus on patient care. Tools like Google Translate aid communication between providers and patients with limited English proficiency, improving care quality. In surgery, AI systems recognize instruments with nearly 90% accuracy, reducing errors and enhancing safety. By automating routine processes, AI helps build a healthcare system centered on patient needs.
Little Transparency
Despite these advances, significant hurdles remain. Many AI systems operate as “black boxes,” offering little transparency into how decisions are made. This lack of explainability undermines clinician trust. Biases in training data further compound risks, as algorithms may perform poorly for underrepresented groups, worsening health disparities. For example, models trained on data from specific demographics might miss critical signs in diverse populations.
Regulatory frameworks also lag behind AI’s rapid evolution. Unlike drugs or devices, AI tools often enter clinical use without rigorous trials proving their safety or effectiveness. This gap raises concerns about accountability—especially when AI influences life-changing medical decisions. Ethical questions about data privacy and patient consent add another layer of complexity. Who is responsible if an AI-driven recommendation leads to harm? How can patient data be used ethically to train these systems?
Also Read: Digital Therapy Shows Promise for Teen Mental Health
Explainable AI
Collaboration is essential to overcoming these challenges. Researchers are developing “explainable AI” to make algorithms more transparent, aligning their logic with clinical reasoning. Efforts to diversify training data and implement real-time bias detection aim to create fairer, more equitable tools. Regulatory bodies are exploring dynamic oversight, monitoring AI performance continuously rather than relying on one-time approvals.
The future of AI in medicine hinges on balancing innovation with responsibility. By prioritizing transparency, equity, and rigorous testing, AI can evolve from a promising tool to a trusted partner in healthcare. This vision demands input from clinicians, ethicists, policymakers, and patients to ensure technology serves humanity’s needs.
As AI reshapes healthcare, the stakes are high—but so are the opportunities. With thoughtful integration, AI could democratize access to care, reduce clinician burnout, and improve outcomes for millions. The path forward requires more than technical breakthroughs; it demands a commitment to ethics, inclusivity, and collaboration. The promise of AI in medicine is clear—the challenge lies in turning that promise into practice.




