The Unequal Burden of Breast Cancer: A Race Against Time and Inequity
Breast cancer cases reached 2.3 million in 2022, projected to rise 38% by 2050, disproportionately impacting low-income regions. Mortality rates in low-HDI countries are up to five times higher.

AI Research Assistant
Analyze this article instantly
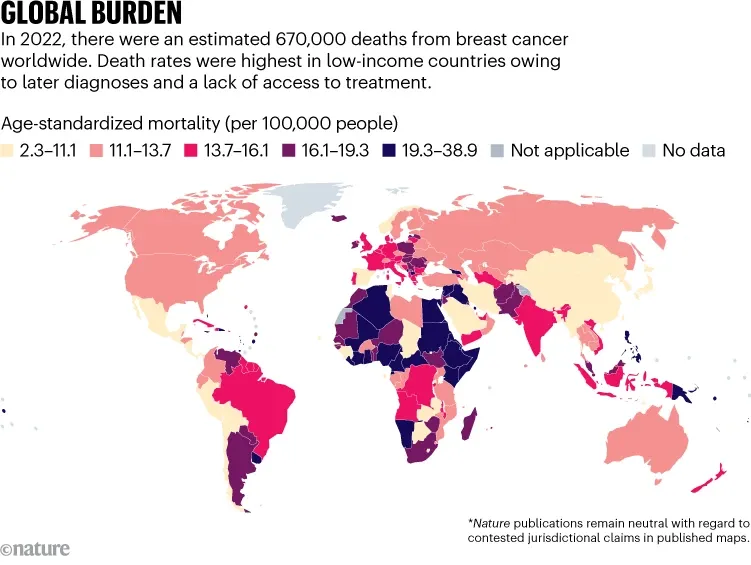
Every minute, four women are diagnosed with breast cancer worldwide, and one loses her life to it. Breast cancer remains the most commonly diagnosed cancer and a leading cause of cancer deaths worldwide, with 2.3 million new cases and 670,000 deaths reported in 2022.
A recent study in Nature Medicine highlights stark global disparities in incidence and mortality rates driven by differences in lifestyle, healthcare access, and socioeconomic development. By 2050, cases are projected to rise by 38% and deaths by 68%, with low-income regions bearing the brunt of this increase.
Unequal Burden
In 2022, breast cancer incidence rates were highest in Australia, New Zealand, and Northern Europe, while mortality rates were worst in Melanesia, sub-Saharan Africa, and parts of Asia. High-income countries with advanced healthcare systems saw better survival rates, but low-income regions struggled with late diagnoses and limited treatment access. For example, mortality rates were 56% of incidence rates in low-development countries, compared to just 17% in high-development nations.
Rising Cases in Rapidly Developing Nations
Over the past decade, breast cancer incidence rose sharply in countries like Bahrain (+4.8% annually), South Korea (+4.6%), and Japan (+4.2%), linked to lifestyle changes such as later childbirth, less breastfeeding, and rising obesity. Meanwhile, mortality rates dropped in many high-income nations, including Belgium, Denmark, and Switzerland, which met the World Health Organization’s (WHO) target of reducing breast cancer deaths by 2.5% yearly.
A Growing Crisis
By 2050, breast cancer cases are expected to hit 3.2 million globally, with deaths reaching 1.1 million. Low-income regions will face the steepest increases—165% more cases and 161% more deaths—due to ageing populations, rising risk factors, and inadequate healthcare infrastructure. Younger women in these areas are particularly vulnerable, as nearly half of breast cancer cases in Africa already occur in women under 50.
Equity in Care
The study urges governments to prioritize early detection, affordable treatment, and prevention strategies. While high-income countries benefit from screening programs and advanced therapies, low-resource settings need scalable solutions like clinical breast exams and targeted public health campaigns. The WHO’s Global Breast Cancer Initiative aims to reduce mortality by 2.5% annually, but progress remains uneven.
Up to a quarter of breast cancers could be prevented through lifestyle changes: reducing alcohol, maintaining a healthy weight, and promoting breastfeeding. Global collaboration is critical to address inequities, strengthen cancer registries, and ensure no region is left behind in the fight against this disease.




